2022 Healthcare Trends: Adapting to Changing Patient Needs
The past several years have been dramatic for the pharmaceutical industry as the number of specialty therapies on the market continue to rise- in...
3 min read
 CareMetx
:
Sep 30, 2021 10:47:41 AM
CareMetx
:
Sep 30, 2021 10:47:41 AM

When infusion centers deliver life-saving treatments, they need to ensure those treatments are accessible and affordable for all patients- while also ensuring their practice will be reimbursed appropriately upon delivering them. In the complex world of health insurance, that’s easier said than done.
Greg Morris, CareMetx Chief Strategy Officer, recently discussed these challenges as a guest on the WeInfuse podcast. Greg explained the drivers leading infusion practices to streamline their processes using hub services, and how this technology is improving the patient experience while providing practices with greater reimbursement certainty.
Navigating the complicated health insurance landscape takes the kind of time and energy that patients with life-threatening diseases simply don’t have. But unless their insurance benefits are verified and they receive prior authorization when it’s required, they could be denied infusion treatments—or worse, face a daunting bill they don’t have the resources to pay.
“Even if an insurer covers 80 or 90 percent of an infusion treatment- when the therapy costs as much as $5,000 a month, the patient’s share still amounts to a lot of money,” Greg explains.
That’s why obtaining the necessary benefits verifications and prior authorizations in a timely way is critical to infusion center owners and operators. It makes the difference between the patient starting treatment right away or facing delays, and it determines whether the practice is reimbursed fully or is left with a shortfall- one that could amount to tens of thousands of dollars.
Greg also notes that two interrelated challenges pose risks for infusion centers and their patients: treatment affordability and operational inefficiency.
|
|
Treatment Affordability- While infusion center operators are often aware of resources patients can lean on for financial help- things like manufacturer co-pays- the navigation of said resources isn’t always simple. For example, medicare patients aren’t eligible for those co-pays, yet they may qualify for low-income government subsidies instead. “There may also be public or manufacturer foundations the patient can access for funding,” Greg continues. Given that affordability is a widely known obstacle to a patient’s adherence to treatment, removing these financial barriers is vital. |
|
|
Operational inefficiency- Operational inefficiency can also get in the way of an infusion center’s ability to deliver these life-altering therapies. Onboarding patients and ensuring they have treatment access has historically involved a complicated, time-consuming manual process—from enrolling the patient, to capturing consent, verifying benefits, and ultimately getting a prior authorization. At every step, delays and errors can occur. Multiply that process across the many therapeutic brands a typical infusion center works with, and the risks grow exponentially. “The infusion practice typically has to contact different call center teams for every brand—even different brands from the same manufacturer,” Greg says. This creates tremendous “portal fatigue” and can increase the odds of delays and mistakes that neither the infusion center nor the patient can afford. |
To solve these issues, many infusion practices are turning to hub services technology that connects specialty pharmaceutical manufacturers, patients, and providers. By embedding patient access services directly into their workflow, infusion centers are adopting a simpler, more streamlined process that benefits everyone involved.
“Infusion centers that use hub services know they’ll get paid for the therapies they administer, so they gain greater reimbursement certainty,” Greg notes. “The center is confident the patient can afford the therapy long term, and the provider is confident the patient will adhere to the treatment plan, which improves outcomes.”
The difference between a manual process and one automated with hub services can be stark: End to end, a manual process takes one to three hours of staff time, with prior authorizations sometimes taking one or two weeks to come through. When the process is automated, the staff might spend only 10-15 minutes on the same tasks.
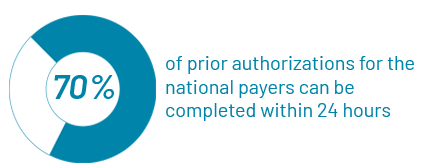
“More importantly, about 70 percent of prior authorizations for the national payers can be completed within 24 hours,” Greg says. “When patients can get on therapy a week or two sooner, that’s a game changer.”
As with any change, moving from a manual onboarding and verification process to a technology-based approach may be met with resistance. To pave the way for success, Greg recommends these best practices:
In the end, infusion practices will continue to play a critical role in delivering essential specialty treatments to patients with life-threatening diseases.
And perhaps it’s true that the complexities of the healthcare landscape aren’t likely to subside anytime soon. But by streamlining these processes through technology, infusion center owners and operators can improve patient access to affordable care and ensure their practice is properly reimbursed.

The past several years have been dramatic for the pharmaceutical industry as the number of specialty therapies on the market continue to rise- in...

Specialty care is traditionally high-touch. With patients, caregivers, nurses, case managers, field reimbursement managers, and more, there are a lot...

Specialty medications provide hope for hundreds of thousands of patients in the United States, but this hope often comes at a high cost, in terms of...