How Annual Benefit Changes Can Negatively Impact Patient Adherence
We’re in the midst of benefits reverification season- a time when physicians and specialty pharmacies tackle the time-consuming task of confirming...
5 min read
 CareMetx
:
Sep 7, 2021 5:00:24 PM
CareMetx
:
Sep 7, 2021 5:00:24 PM

Specialty pharmaceuticals are a rapidly growing form of treatment that shine a uniquely bright light on a mounting need for practical, user-friendly digital healthcare solutions for all stakeholders throughout the care process. Typically used to treat chronic, serious, or life-threatening conditions such as cancer, “specialty pharmaceuticals” refer to treatments that have been classified as:

As of July 2021, 36% of total pharmacy revenue could be attributed to specialty pharmaceuticals like these.
Looking forward, of around 7,000 prescription drugs currently in development it is estimated that specialty medications account for 5,250 - that’s 75%. The global market size of home infusion therapy alone is projected to reach $29,640 million by 2027, a 5.8% compound annual growth rate leap from $19,850 million in 2020. The market for infusion-specific ambulatory centers is currently worth nearly US$ 47 million, and is estimated to witness a CAGR of 9.0% over the next 6 years, driven largely by consistently rising cases of cancer in the US.
We are clearly seeing a seismic shift toward a reliance on this type of specialty therapy care, and it should come as no surprise. In the year 2020, it is estimated that 1,806,590 new cases of cancer will be diagnosed in the United States, and 606,520 people will die from the disease. As millions of Americans continue to suffer from illnesses that require more intense, high-touch, and complicated care, leaders within the healthcare industry will increasingly face pressure to make more practical choices in optimizing therapy and drug distribution methods in order to provide these ailing Americans with the care they need, at scale, and at the rapid pace these life threatening illnesses demand.
This complex care influx will surely steer a strong industry focus on the implementation of more straightforward, provider-friendly technology solutions and manufacturer distribution models that properly serve all stakeholders- the providers, patients, manufacturers, and payors alike. Put simply, a seismic shift towards specialty care has begun to pull back a curtain on the healthcare industry’s failing reliance on antiquated methods such as phone calls and faxes, and a mounting need to better meet today’s digital standards.
Providing effective treatment to patients with complex diseases is inherently challenging to stakeholders throughout the process for a number of reasons. But if providing the best possible care for patients is truly central to the mission of our pharmaceutical and healthcare leaders, a focus on the experience of these patients themselves should lead the conversation around how to optimize as we map out the future of care.
The sobering reality is that thousands of patients who suffer from life-threatening illnesses never wind up receiving the care they need, even when their providers know exactly the therapy plan required to treat the illnesses they suffer from. Information on nonadherence (patients who do not take prescribed medication or follow course of treatment) of this nature is widely available across specialty and non specialty medications- however these figures are often determined using pharmacy claims data alone, which may not effectively capture the full picture of adherence rates for care plans as complex as specialty therapy ones.
In 2019, Journal of Managed Care & Specialty Pharmacy conducted a single center, retrospective cohort study in order to better understand the issue of nonadherence amongst patients who are specifically prescribed specialty medications. Through their methods, electronic medical records of a random 10% sample of patients deemed nonadherant were manually reviewed to identify reasons for nonadherence. What they found was that of 7,488 records from 18 specialty areas sampled, 1,059 met the criteria for nonadherence. Once a 10% percent random sample of this cohort was identified and said sample was reviewed, it was found that 58% were truly nonadherent.
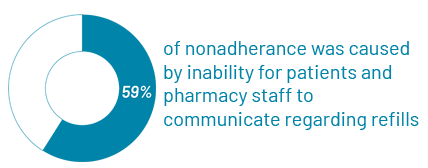
Per their findings, the most common cause of true nonadherence was a communication barrier- the inability for patients and pharmacy staff to communicate regarding refills. This accounted for 59% of nonadherant patients sampled. Other top reasons for nonadherence identified were low health literacy (16.4%), patient unresponsiveness (16.4%), and financial barriers (16.4%).
The realities of these financial barriers and communication back-and-forths were sadly illustrated through a conversation with Molly D'Aulerio, who has been working as a case manager coordinating home health aide care since 2017. The care Molly coordinates specifically specializes in providing at-home care services to elderly, terminally ill and disabled individuals- many of whom rely on specialty therapies to treat their illnesses.
Molly describes the frustration and confusion her patients and their families experience when faced with little support or guidance while coordinating things like confirming benefits verifications and making sure these specialty therapies are authorized.
"It feels incredibly unfair to expect these patients and families- who are already under a great deal of stress from the knowledge alone that their loved one is critically ill and dying- to manage all these insurance back and forths while they're kept waiting to receive access and start on the specialty medication plan," she shares.
"Something seriously needs to change within the industry, because the way it works now is unnecessarily cumbersome and confusing for the patients, who are really too sick to be dealing with that added burden whatsoever. These patients deserve a faster, more straightforward experience- from when they’re prescribed their therapy plan, to when they get access to it and can get started."
Clearly, if pharmaceutical and healthcare leaders seek to eliminate barriers to specialty care for patients, a focus on efficient therapy distribution, straightforward, expedited care, and innovative patient engagement and communication methods would seem a practical place to start. That’s where more practical digital healthcare solutions have the opportunity to play a critical role.
When we examine barriers to care such as the aforementioned delays caused by prior authorization back and forths, it’s important to take a look inside the struggles within the workflow of the care provider and pharmacist as well.
Physicians often express equal frustration with the barriers and delays repeatedly presented by standard prior authorization processes. In Texas, a new law is currently being introduced that states doctors who have a strong track record of getting the greenlight from insurance companies will no longer have to obtain prior authorization from health insurers at all.
The Federal government seems to agree with a need to address this provider frustration. In May 2021, Representatives Ami Bera, M.D. (CA-07), Suzan DelBene (WA-01), Mike Kelly (PA-16), and Larry Bucshon (IN-08) introduced bipartisan legislation that would make prior authorization in Medicare Advantage plans less burdensome by establishing an electronic approval process and a real-time decision process for items that are routinely approved.
Measures like this- standardized electronic approval processes, real-time medical care initiated by automation and more efficient technology- is at the heart of what non-dispensing specialty pharmacies seek to provide. By leveraging electronic health records access along with the ability to engage directly with physicians, non-dispensing specialty pharmacies offer the much more efficient, high-touch coordination of care that these complex illnesses require. To quote the aforementioned Journal of Managed Care & Specialty Pharmacy study, “Research shows higher adherence rates in patients using a specialty pharmacy compared with a retail pharmacy.”
Non-dispensing specialty pharmacies have a great ability to expedite prescription dispensing through the use of automation and proprietary technology that physicians can imbed directly into the native workflows that they are already comfortable using. By speeding this access to care, we see benefits to stakeholders across the spectrum- to the physicians and pharmacists who no longer have to wrangle with red tape and prior authorization back and forth, to the manufacturers who can more readily distribute their therapies, and most importantly- to the patients who are no longer kept waiting for the care they need.
If leaders across the healthcare and pharmaceutical industries truly seek to provide patients with top tier care, digital coordination and real-time processes like these should indisputably be our standard. Throughout the coming years, the healthcare and pharmaceutical industry will face mounting pressure to meet said digital standards that allow for more efficient, straightforward care. From the legal and regulatory changes being pushed at both state and federal level to the daily frustrations shared by caregivers and patients, this demand for the industry to rise and meet the challenge of a new digital standard will surely continue to grow by the day.

We’re in the midst of benefits reverification season- a time when physicians and specialty pharmacies tackle the time-consuming task of confirming...

The past several years have been dramatic for the pharmaceutical industry as the number of specialty therapies on the market continue to rise- in...

Specialty care is traditionally high-touch. With patients, caregivers, nurses, case managers, field reimbursement managers, and more, there are a lot...