How Annual Benefit Changes Can Negatively Impact Patient Adherence
We’re in the midst of benefits reverification season- a time when physicians and specialty pharmacies tackle the time-consuming task of confirming...
2 min read
 CareMetx
:
Oct 21, 2021 4:53:01 PM
CareMetx
:
Oct 21, 2021 4:53:01 PM

We’re quickly approaching a time of year that too-often overwhelms many stakeholders throughout the healthcare industry: insurance reverification season- known to some as blizzard season.
While the thought of tackling this annual reverification process may bring a sense of dread to some organizations, many leaders are finding that the right approach coupled with the right technology is helping them tackle this annual challenge both efficiently and painlessly— all while improving patient adherence and treatment outcomes.
Between November and January, most health insurance plans institute policy changes, sometimes adding or removing which services they cover.
At the same time, patient deductibles and out-of-pocket maximums reset for the new benefit year. Though it happens annually, patients aren’t always prepared for the changes that will go into effect. That can prove problematic for providers and patients alike—especially those receiving specialty treatments.
At some point during the year, once patients satisfy their annual deductibles and reach their out-of-pocket thresholds, they start to receive treatments and prescriptions at no cost. But when each new benefit year begins, said patients find their deductible threshold meter has “reset” so to speak- resulting in unexpected out-of-pocket charges. Worse, they may be denied access to healthcare services until a new prior authorization is received, thus delaying their access to potentially life-saving treatment. Additionally, if patients who use financial assistance programs need to re-enroll each year but don’t remember to do so, they could be left with medical bills they simply can’t afford.
For manufacturers looking to streamline this process and avoid aforementioned disruptions, ensuring that the annual insurance reverification season goes smoothly for your brand requires a methodical approach.
By following proven best practices gleaned from CareMetx’s track record of conquering blizzard season on behalf of our clients, you can minimize the disruption caused by reverification season, get through this challenging time more effectively and efficiently, and help keep your patients on their treatment.
Handling a high volume of reverifications manually is time consuming and error prone. Technology that connects specialty pharmaceutical manufacturers, patients, and providers speeds the process and improves accuracy. CareMetx Digital Hub is a comprehensive platform for addressing the complexities of specialty reimbursement.
Learn more about CareMetx Hub Services.
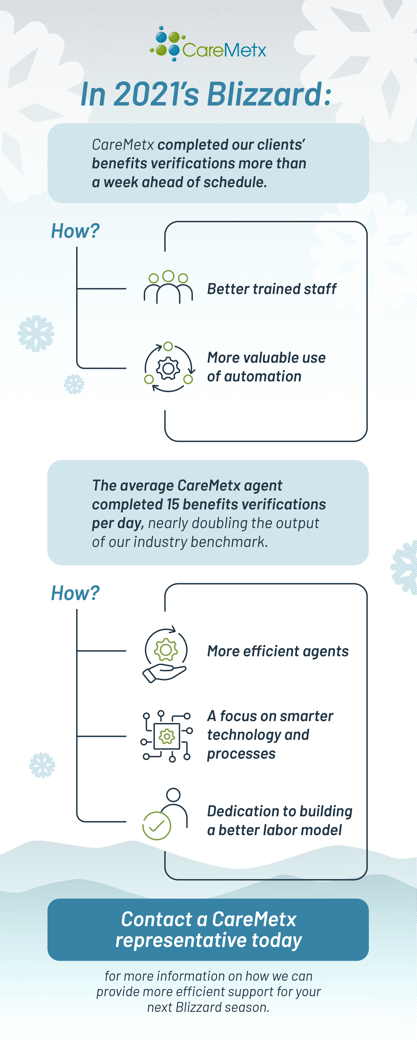
“CareMetx is the industry leader in automated Benefit Verifications,” shares CareMetx Chief Strategy Officer Greg Morris.
“Our proprietary process combines our extensive payer connectivity and rules engine with specialized benefit verification team members to generate scalable benefit verification results that are consistently 2x more efficient than industry standards.”
Learn more about CareMetx’s eServices.
Learn more about CareMetx Benefits Reverification Support
It’s time to take the chaos and uncertainty out of reverification season- for manufacturers, for providers, and most importantly- for patients.
For leaders who are ready to improve the insurance verification and prior authorization process—both during blizzard season and year-round, contact CareMetx to learn about the hub services technology that’s helping leading organizations streamline these processes every day.

We’re in the midst of benefits reverification season- a time when physicians and specialty pharmacies tackle the time-consuming task of confirming...

Specialty care is traditionally high-touch. With patients, caregivers, nurses, case managers, field reimbursement managers, and more, there are a lot...

Specialty medications provide hope for hundreds of thousands of patients in the United States, but this hope often comes at a high cost, in terms of...