Why Hub Services Data is Increasingly Valuable to Pharmaceutical Manufacturers
Accurate, transparent data is quickly becoming a critical piece of pharmaceutical manufacturers’ decision making processes. To ensure patients have...

When a patient has a serious or complex health problem that needs attention, the journey to receive a diagnosis and obtain the right specialty therapy can be complicated and frustrating. Fortunately, the right hub services technology can eliminate their pain points and smooth the path to receiving life-altering treatments.
Examining a Use Case: It Starts with Schedules and Paperwork
To examine a common patient journey, first a patient calls their healthcare provider (HCP) to schedule an appointment. As a new patient, they’re asked to provide their health insurance information to ensure the appointment will be covered. Once the HCP and insurance company confirm that the patient is eligible for the appointment, the enrollment period begins.
Next, the patient arrives at the appointment 15 minutes early as requested to fill out the necessary paperwork. They are handed a bundle of papers on a clipboard (or they might be given an electronic tablet), then they start the time-consuming process of completing, signing, and dating each section, along with an informed consent form typically. The informed consent form is designed to protect the patient by ensuring the physician provides any information needed to make decisions about tests, procedures, treatments, and payments.
The patient returns the completed forms to the front desk, and is eventually brought to the exam room to meet with the doctor. In the meantime, the enrollment process continues behind the scenes as the data from the paperwork is entered into a system and becomes part of an electronic healthcare record (EHR).
It Moves on to Diagnoses and Approvals
After a series of tests, the physician informs the patient that they have a medical condition that is treatable with a specialty medication. However, the therapy is relatively expensive and isn’t available at a local pharmacy. To access this therapy, the patient will need to visit the physician’s office or a treatment center on a regular basis for treatments.
But that’s just the start. Although the patient has health insurance, this unique medication needs to be approved by their insurer before being dispensed. This is where the process can really get bogged down- even if the insurer approves the medication, the prior authorization (PA) process can be slow. Eventually, the patient may start to wonder: How long will it take for my insurer to approve this treatment? What will the out-of-pocket cost be? What if I can’t afford it? Enter CareMetx.
Technology Speeds and Simplifies the Journey
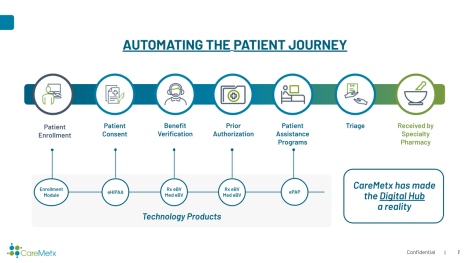
CareMetx improves the patient journey to specialty therapies by combining radically efficient, proprietary technology with a customer support staff focused on driving the patient’s speed to therapy. From the patient intake and enrollment process to the delivery and administration of the medication, the CareMetx solution and customer support team is tightly integrated with the HCPs and pharmaceutical manufacturers that impact the patient’s journey—speeding the approval process so patients can access much-needed treatments faster.
Right from the start of the patient intake and enrollment process, CareMetx is hard at work behind the scenes, safely and securely capturing the patient data the HCP enters. When the enrollment form is completed via the CareMetx Enrollment Module, it triggers the next steps, including benefit investigation and PA. The data collected also can be used to populate additional forms—such as informed consent or a co-pay or patient assistance program (PAP) form—to speed the process, streamline the workflow, and minimize data entry errors.
While the payer is reviewing the PA for medication reimbursement purposes and approving it, denying it, or requesting more information, the pharmaceutical manufacturer might offer the HCP a free shipment of a startup or bridge drug if the authorization process gets delayed.
Throughout this streamlined digital enrollment process, the CareMetx Connect HUB also provides a human touch. Our Connect staff monitors the process to ensure each step is completed quickly and accurately, and they’re just a phone call away if questions arise.
Once the payer approves the treatment, the Connect team combines all the approval forms into a triage package and submits it to the dispensing pharmacy via the CareMetx portal HUB based on the patient’s benefit design. The dispensing pharmacy is automatically notified of the triage packet and dispenses the therapy to the HCP, the CareMetx HUB system is updated to reflect that the drug has been dispensed, and the HCP contacts the patient to schedule the therapy.
The CareMetx digital hub platform can initiate, facilitate, and track every step and service in the patient journey, providing a portal that helps HCPs, insurance companies, and pharmaceutical manufacturers reduce the lengthy, time-consuming specialty therapy approval process from weeks to just days. And that means patients can get life-altering treatments faster, improving their health outcomes and their quality of life.

Accurate, transparent data is quickly becoming a critical piece of pharmaceutical manufacturers’ decision making processes. To ensure patients have...

The past several years have been dramatic for the pharmaceutical industry as the number of specialty therapies on the market continue to rise- in...

Think beyond patent expiration to maximize brand value throughout your therapy’s life cycle Your drug is launched and is gaining recognition. You’re...